Greetings,
The statute has an inconsistency in addressing when a response to a Petition for Benefits is due. Under 440.192(8), the carrier must respond to the PFB within 14 days. However, under 440.34(3)(d) no attorney fees are due to the claimant’s attorney as long as the response is done within 30 days. (Both statutes are below).
Why this is important is that sometimes you don’t know the answer to whether or not you owe the benefits within 14 days after the PFB was filed…and if you respond with an equivocal or vague response on the PFB you may owe attorney’s fee. In some circumstances, you may need that extra 16 days (total 30 days) to make the correct decision.
(I have heard from clients that the Division of WC does monitor/penalize the 14 days response timeframe, and some carriers require the adjusters comply for that reason.)
Two examples of where this often comes into play are a claim for payment of medical bills and a request for surgery that needs to first go through the pre-certification process.
A response to a PFB for payment of an emergency room or other medical bill that says “the medical bills will be paid per fee schedule when received on proper form if casually related” is not a provision of the benefit because of the ending phrase. That basically means maybe we will pay or maybe we won’t. Understandably we can’t simply agree to pay a bill if we don’t know what was treated. You should immediately request the bills and the records to see what was done.
An alternative way to do it is to state “any and all treatment for the compensable body parts (list them) on the attached bills will be paid per fee schedule and the E/C has requested it be placed on proper form for payment.” Just one suggestion. I have also seen fee entitlement in this situation if the bill remains unpaid after several months, and the E/C has not requested the bills on proper form. So, find a way to answer that the bills we be paid, then take steps to get them paid.
As for surgeries that have to go through a pre-certification or peer review process, let the person handling that process know your deadlines. If you get a response the surgery is certified on day 31 you owe a fee.
If you don’t think you will be able to make the decision within 30 days, look to see if there are grounds to have the PFB dismissed for lack of specificity or failure to attach the evidence that supports the claimed benefits. You only have 30 days to file a Motion to Dismiss from when the PFB was filed, see 440.192(5) below. It is also possible to file a Motion to Dismiss for failure to make a good faith effort to resolve the issues before filing the PFB, but these are difficult to prove. In reviewing the JCC decisions from around the state, I am not seeing a lot of success to this tactic.
Thanks, and let me know if you have any questions.
Sincerely,
Morgan Indek | Partner
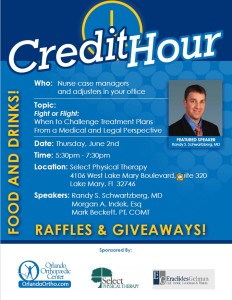
Please join me on 6/2/16 for a Credit Hour with Dr. Randy Schwartzberg from Orlando Orthopaedic at 5:30 in Lake Mary (flyer attached). The topic is Flight or Fight; when to challenge medical treatment plans. Please RSVP to esantos@eraclides.com
(Click to Enlarge)